Inflammatory Bowel Disease: Symptoms, Types, Diagnosis and Treatment Options
Inflammatory Bowel Disease (IBD) is a group of chronic conditions characterized by long-term inflammation of the gastrointestinal (digestive) tract, caused by an abnormal immune response.
Inflammatory Bowel Disease (IBD)
Patient Information & Education
Inflammatory Bowel Disease (IBD) refers to a group of chronic conditions in which the body’s immune system causes ongoing inflammation of the digestive tract. These conditions typically follow a relapsing and remitting course, with periods of symptoms alternating with periods of relative well-being.
IBD is not an infection, it is not contagious, and it is not caused by stress alone, although stress may worsen symptoms. With appropriate medical care and follow-up, many patients with IBD are able to lead active and productive lives.
Types of Inflammatory Bowel Disease
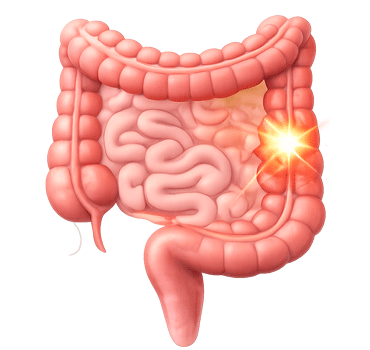
Ulcerative Colitis
Ulcerative colitis affects the large intestine (colon and rectum). The inflammation is continuous and limited to the inner lining of the bowel.
- Bloody diarrhea
- Urgency to pass stools
- Urgency to pass stools
- Mucus in stools
- Lower abdominal pain

Crohn’s Disease
Crohn’s disease can affect any part of the gastrointestinal tract, from the mouth to the anus. Inflammation may involve the full thickness of the bowel wall and often occurs in a patchy distribution.
- Abdominal pain
- Diarrhea, with or without blood
- Weight loss
- Perianal disease such as

Why Does Inflammatory Bowel Disease Occur?
IBD develops due to an abnormal immune response in genetically susceptible individuals. Instead of protecting the intestine, the immune system reacts excessively and causes persistent inflammation.

Genetic predisposition

Altered gut bacteria

Environmental triggers

Smoking
Common Symptoms
Symptoms vary depending on the type, location, and severity of disease. They may include:

Chronic diarrhea

Blood or mucus in stools

Abdominal cramps or pain
Fatigue and anemia

Weight loss
How Is Inflammatory Bowel Disease Diagnosed?
There is no single test that confirms IBD. Diagnosis is made by correlating clinical findings with investigations.
Evaluation may include:
- Detailed medical history and physical examination
- Blood tests to assess inflammation and anemia
- Stool tests such as fecal calprotectin
- Colonoscopy
- Imaging studies such as CT or MRI enterography when required

Treatment of Inflammatory Bowel Disease

Treatment is individualized and depends on the type of IBD, disease extent, severity, and response to therapy. The goals of treatment are to control inflammation, achieve and maintain remission, and prevent complications.
- Medical management may include:
- Anti-inflammatory medications
- Immunomodulatory drugs
- Biologic therapies
- Nutritional and supportive care
Patients with long-standing colonic disease may require regular 🔗 surveillance colonoscopy
Living With Inflammatory Bowel Disease
With appropriate treatment and regular follow-up, many patients with IBD are able to live full and active lives.
Important aspects of long-term care include:
- Adherence to prescribed medications
- Regular medical follow-up
- Nutritional optimization
- Vaccinations when indicated
- Surveillance colonoscopy as advised
Frequently Asked Questions
Is inflammatory bowel disease curable?
Inflammatory bowel disease is a chronic condition. While there is currently no permanent cure, modern medical and surgical treatments can effectively control inflammation and help patients remain in long-term remission.
Is IBD the same as IBS?
No. IBD involves chronic inflammation and structural damage to the bowel, whereas irritable bowel syndrome (IBS) is a functional disorder without inflammation or bowel damage.
Does everyone with IBD need surgery?
No. Most patients with IBD are managed with medications. Surgery is required only in selected situations such as complications or failure of medical treatment.
Can diet alone treat IBD?
Diet alone does not treat IBD. However, dietary modifications can help control symptoms and improve nutritional status when combined with medical therapy.
Does IBD increase the risk of colorectal cancer?
Yes. Long-standing inflammatory bowel disease involving the colon increases colorectal cancer risk, which is why 🔗 regular surveillance colonoscopy
About the Author of This Information
Dr. Rajeev Kapoor is a practicing surgeon based in Mohali, Punjab. He provides clinical services in the field of gastrointestinal, colorectal, and general surgery. This website is intended for informational and educational purposes only.
Disclaimer
The educational content has been authored for patient awareness and public health education. It does not constitute solicitation or promotion of medical services



